All You Should Know About Cervical Cancer
It’s hard to find words to describe what was undoubtedly, one of the most unsettling, yet enlightening 30 minutes I’ve experienced this year. I am still a bit shaken.
A word of caution: if you have a low threshold for sorrow, for the sake of your emotional health (and so you don’t drown your mobile device in a pool of tears), here’s your chance to stop reading before it’s too late.
The hospital environment is usually a place of hope; most people who check in ill, check out well. On this fateful day, I met Pat. Pat wasn’t looking too hopeful. When I walked into the Gynaecology Ward around 9am, I spotted her lying almost motionless in a bed at the extreme end of the left wing, with her face to the ceiling. I caught her a few times, wince with pain. As I slowly sank into a wood-framed cushioned chair beside her, I could tell she had fought this for a while already. It was also obvious that this illness dealt some really hard punches. Pat, who looked like she was in her mid-fifties, must have been admitted from the previous night shift, because I knew so little about her. I noticed however, that her collar bones were prominent. And so were the bones on her face. We spoke for a while and she told me about her frequent vaginal bleeding, even though she had hit menopause like two years ago. She spoke of her 6 children at home and how she loves them so much. Pat told me about her husband, who left her a few months ago because he got tired of paying her huge recurring medical bills. It wasn’t long that I deduced what was wrong with Pat: She had cancer of the cervix.
HERE’S WHAT YOU SHOULD KNOW ABOUT CERVICAL CANCER
A lot of us already know that the word “cancer” suggests something that should be of great concern. The cells in our body have to divide and replicate in an orderly and controlled manner in order for us to function optimally. When this process goes haywire, it’s called cancer.
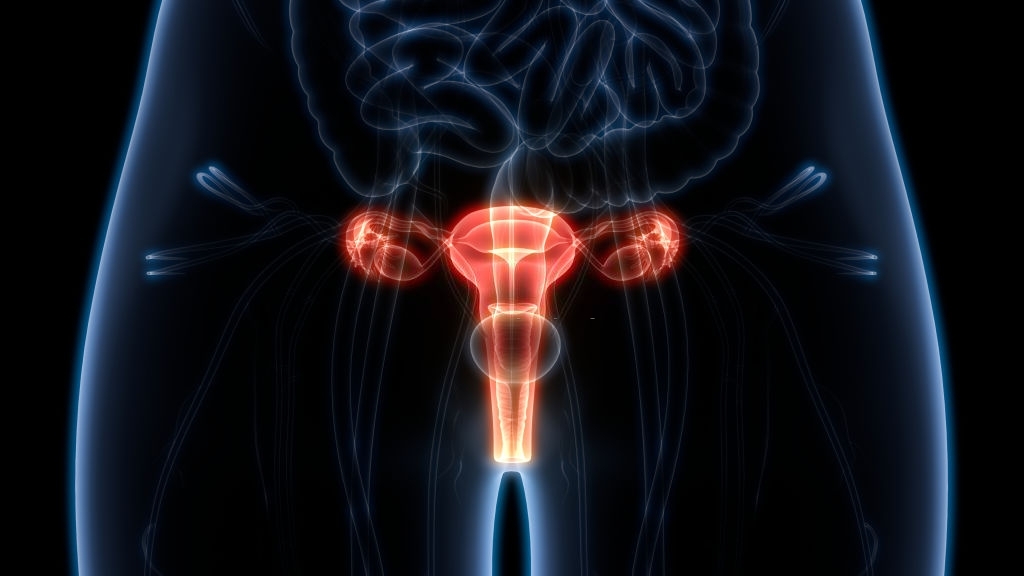
Cancer can affect any part of the body. In Pat’s case, it affected her cervix. The cervix is a cylindrical mass of tissue that connects the womb and the vagina.
Globally, cancer of the cervix is the second most common cancer affecting females; the first being breast cancer. In developing countries like Nigeria, cervical cancer ranks number one, mostly due to poor screening habits.
WHAT CAUSES THIS KIND OF CANCER?
It’s not yet certain what actually causes cervical cancer. There are however, certain risk factors associated with this disease. The most important is the infection with a virus known as “Human Papilloma Virus”, most especially the highly virulent strains which are simply denoted by the numbers ‘16’ and ‘18’ respectively. Let’s take a look at the risk factors that were obvious in Pat:
- Multiple child birth, which is also referred to as “high parity”. Pat told me that she had 6 children. Here’s a rule of thumb: when you’re on your 5th pregnancy, you’re already doing too much.
- Pat is black. Research shows that cervical cancer is fairly common in Africans. It seems like even diseases are racist these days.
There are a couple of other factors that increase the risk of getting this cancer:
- Initiating sexual intercourse at an early age
- Involvement with several sexual partners
- Having a sexual partner who has numerous sexual partners
- Lowered immunity which may be caused by HIV/AIDS infections, prolonged steroid use, cigarette smoking, etc
- It is common in the lower socio-economic class
- Cancer of the cervix is common with certain families
Of course, having these risk factors does not automatically spell doom. It only means that this group of women have a higher chance of coming down with this cancer when compared with the rest of the population.
HOW CAN YOU TELL WHEN SOMEONE HAS CANCER OF THE CERVIX?
When I spoke to Pat, there were two important symptoms that pointed to cervical cancer:
- Vaginal bleeding. But Pat didn’t complain of just any kind of vaginal bleeding, she was having the kind of bleeding that comes even after menopause. This is what is known as post-menopausal bleeding. Cervical cancer could also manifest as bleeding immediately after having sex or bleeding in between menstrual periods.
- Weight loss. Pat’s collar bones were prominent. That suggests that she had lost a lot of fat and muscle mass. Weight loss isn’t specific for just cervical cancer, it is common with many cancer types. Weight loss in a woman like Pat would only make you more suspicious that she indeed had cancer of cervix.
Other symptoms that would increase your suspicion:
- Vaginal discharge which may be whitish and may have an awful smell
- Pain which may be over the abdomen, on the back, in the pelvis or the chest, depending on the degree of spread of the cancer cells
- Pain during urination, urinating more often and uncontrollable urination, could be present. These symptoms suggest that the cancer is spreading and has invaded the bladder which lies close to the cervix.
- Swelling of the leg, which in medical terms, is known as pedal oedema. A drainage system known as a lymphatic channel gets blocked which causes the fluid it carries (lymph) to accumulate in the leg involved.
- Loss of appetite. Again, this is found in a lot of cancer types.
It’s not also unusual for cervical cancer to be associated with no symptoms whatsoever, and only get diagnosed during a routine screening test.
HOW CAN IT BE PREVENTED?
The easiest way to prevent cervical cancer is to learn, learn some more, and keep learning about it. I’ve saved you a lot of research time already.
There are two other important ways of fighting this:
- There is a vaccine available that helps prevent Human Papillomavirus infection, which by extension, reduces the chances of having cancer of the cervix. Most medical authorities advise that the vaccine be administered between the ages of 9 to 13 years or before sexual exposure.
- Pap test. Pap is short for Papanicolaou, which is the name of the Doctor who invented this procedure in the 1920s. This involves getting cells from the surface of the outer cervix (ecto-cervix) using a small brush and an instrument known as a “spatula”, which is done after widening the opening of the vagina using an instrument known as a “speculum”. This procedure may be a bit uncomfortable but it’s usually painless. This may be done routinely depending on your Doctor’s request.
The specimen gets analyzed in the laboratory. If cells are found to be abnormal, another test called “colposcopy” is done, which involves viewing through the vaginal opening using a colposcope that provides good magnification.
It may be a little late for Pat, but not for you. Let’s fight this!
HOW IS IT TREATED?
Treatment options depend on the exact stage of the disease. As for Pat, the disease is already really advanced. Pat whispered into my ears that she would love to spend more time with her kids when she gets better. Modern medicine may be able to buy her a few years. From my little talk with her, I get the feeling that those years would be pretty fulfilling.

